Alzheimer’s dementia (AD) is the sixth leading cause of death among Americans. It currently affects 5.8 million people. As is the case with autoimmune disease, ⅔ of people with Alzheimer’s in the United States are women. More concerning, current projections suggest that AD will continue to increase. Some estimates indicate nearly 14 million cases by 2050. Even worse, the cause of the disease is unknown and there is no cure. However, new research on the oral microbiome suggests that a cure for Alzheimer’s disease may lie in the mouth.
What is Alzheimer’s Disease?
Alzheimer’s dementia is often first diagnosed after a patient’s loved ones notice severe forgetfulness. For instance, this may include lost objects, lack of attention to hygiene, confusion or a mood shift towards anger or depression. Since Alzheimer’s affects thinking, memory, and behavior it interferes greatly with daily life. Alzheimer’s is a progressive disease, meaning it gets worse over time. Eventually, patients forget how to talk, walk, eat and drink. As the disease advances, they may sleep only a few hours at a time, so they require constant care and attention.
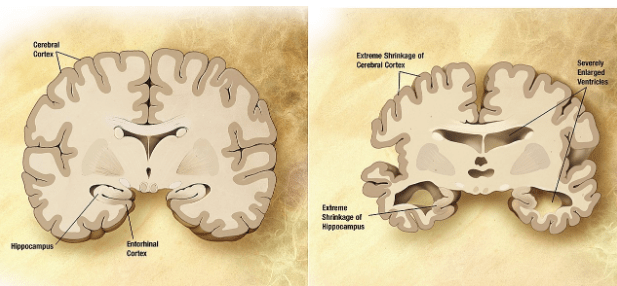
Alzheimer’s is the most common form of dementia. It is a neurodegenerative disease that impairs cognitive function. It’s hallmarks are amyloid-beta plaques, neurofibrillary tangles, and neuronal death. It can only definitively be diagnosed after death, but is usually not the direct cause of death. Most people with Alzheimer’s die of pneumonia or another kind of infection, most likely due to their weakened immune systems.
Is Alzheimer’s a disease of civilization?

Epidemiological research shows that rates of AD have greatly increased over the last 100 years. Of course, many of us alive today would not have been alive 100 years ago. This is because of better nutrition, public health, vaccines and antibiotics. Furthermore, more people live to old age than ever before in human history. Thus, these factors may contribute to the growing incidence of AD.
However, the way we live in modern times differs greatly from how we evolved to live. Because of this mismatch, it is possible we are susceptible to diseases that may not have been prevalent in our evolutionary history. Alzheimer’s may be one of these. Interestingly, the infamous “Alzheimer’s allele” APOE-4 (E4), is the most ancestral allele. This is further evidence of a mismatch between those genes and our modern environment.
The change in the human microbiome through history
Changes in lifestyles over human history have also affected the microbial buddies we coevolved with. Major environmental and lifestyle transitions have resulted in a shift in the composition of our microbiomes. A plethora of research shows that microbial dysbiosis (a change in the normal composition, resulting in imbalance) connects to systemic diseases and various autoimmune disorders. The debate continues on whether or not Alzheimer’s is truly an autoimmune disease, but inflammation and other immune dysfunctions are certainly present.
Alzheimer’s disease and the mouth
Like many autoimmune and other systemic diseases, evidence also supports a link between periodontal disease, tooth loss, and Alzheimer’s Disease. Multiple studies, in many different places, including Sweden, Japan, and the state of Wisconsin shows this linkage.
- A Swedish twin study showed that people who lost more than half their teeth by 35 were more likely to develop Alzheimer’s. [1]
- A Japanese study found that people who had lost more than half of their teeth by age 50-60 were 2.6 times more likely to get Alzheimer’s. [2]
- In Wisconsin, US, a study done of nuns showed that those who had fewer than ten teeth had a 2.2 times risk of developing Alzheimer’s compared to those with ten or more teeth. [3]
While correlation does not mean causation, it is clear that oral health and oral care connect somehow to Alzheimer’s disease. Therefore, understanding this connection may be very important in shedding light on this disease going forward.

Microbes in the mouth implicated in AD
Porphyromonas gingivalis (P. gingivalis), the bacterial species most likely to produce periodontal disease, has recently been implicated in Alzheimer’s disease. For the first time, researchers in Northern California have been able to suggest causality, not just correlation. After infecting mice with P. gingivalis, the scientists found the same bacteria in the mice’s brains, along with amyloid beta plaques—one of the known hallmarks of Alzheimer’s disease. This group, Cortexyme, is currently working on a way to use this new information to create a possible novel therapeutic intervention for Alzheimer’s. This drug is a molecular inhibitor that may disrupt this harmful connection between the mouth and the brain. [4] Click here to read more about their research and work (see page 88).
Alzheimer’s, diet and periodontal disease
Our modern diets may be influencing and even enhancing our risk for developing Alzheimer’s Disease. It’s important to realize that over the course of our long human history, our diets have changed substantially. To read more on how dietary changes have affected our oral health click here.
Dietary changes may be increasing Alzheimer’s risk through changes in the microbe populations living in the mouth. Eating processed and sugary foods encourages harmful bacteria, such as P. gingivalis, to thrive. Accumulation of harmful bacteria can cause mouth dysbiosis, which can subsequently lead to periodontal disease. Check out our article on dietary tips for a healthy mouth.

Did our hunter-gatherer ancestors get periodontal disease?
Evidence from the archaeological record shows that periodontal disease is relatively new in human history. It seems to emerge around the time of the Agricultural Revolution (roughly 10-12,000 years ago) and then escalates during the Industrial Revolution (roughly 200 years ago). While tooth decay and periodontal disease are rare in archaeological samples from hunter-gatherer populations, evidence appears throughout the transition to agriculture. [5]
Researchers did not find P. gingivalis in the dental remains of pre-agricultural revolution hunter-gatherers. However, they did find that species in the dental remains of farming communities post–agricultural revolution. This also coincides with the increased occurrences of periodontal disease. Similarly, another genus associated with Alzheimer’s disease, Treponema, seemingly emerged in the oral microbiome during this time period as well. The rise of world trade in 1500-1750 and the Industrial Revolution thereafter made processed and refined sugars available to millions of people. Unfortunately, refined sugar promotes enamel demineralization, dental caries, and eventual tooth loss — ALL of which are associated with Alzheimer’s disease.
The future of Alzheimer’s research
The oral microbiome, in general, has been understudied, but it is an up-and-coming field in microbiology, immunology, and evolutionary medicine. It’s easy to obtain samples, sequencing is becoming off-the-shelf, and treatments are being developed from this research.
The future for Alzheimer’s patients seems much brighter if we continue to research and expand our knowledge surrounding the oral microbiome and oral health.
Written by Kacey Haptonstall, MS, Becca Malizia, MS
It’s a wonderful thing when the mentees teach the mentor. My young and talented team combined what they are learning in school with some of the research we do here, enlightening me in the process. Let us know what you think! – DrBonnie360
For further reading from our blog
- Click here for more information on current research on the oral microbiome and Alzheimer’s!
- Dr Bonnie’s presentation at the Microbiome Therapeutics US 2019 conference on the connection between the oral microbiome and systemic diseases.
- More on how oral health and well-being connects to systemic health and well-being.
References:
- Gatz M, Mortimer JA, Fratiglioni L, Johansson B, Berg S, Reynolds CA, Pedersen NL. 2006 Potentially modifiable risk factors for dementia in identical twins. Alzheimers Dement 2, 110–117. (doi:10.1016/j.jalz.2006.01.002)
- Kondo K, Niino M, Shido K. 1994 A case-control study of Alzheimer’s disease in Japan–significance of life-styles. Dementia 5, 314–326.
- Stein PS, Desrosiers M, Donegan SJ, Yepes JF, Kryscio RJ. 2007 Tooth loss, dementia and neuropathology in the Nun study. J Am Dent Assoc 138, 1314–1322; quiz 1381–1382.
- Dominy SS et al. 2019 Porphyromonas gingivalis in Alzheimer’s disease brains: Evidence for disease causation and treatment with small-molecule inhibitors. Science Advances 5, eaau3333. (doi:10.1126/sciadv.aau3333)
- Adler CJ et al. 2013 Sequencing ancient calcified dental plaque shows changes in oral microbiota with dietary shifts of the Neolithic and Industrial revolutions. Nature Genetics 45, 450–455. (doi:10.1038/ng.2536)






1 Comment
Exploring the Oral Microbiome ebook – Your Autoimmunity Connection · November 4, 2019 at 11:47 pm
[…] The oral cavity is home to some 700 different species of bacteria that contribute to one of the body’s most significant microbiomes. New understanding of the oral microbiome is showing that a balanced oral ecosystem of bacteria, viruses, and fungi is not only good for our mouths, but also our systemic health. Imbalances of bacteria in the oral cavity have been linked to chronic diseases such as heart and lung disease, cancer, autoimmune diseases, and even (possibly) Alzheimer’s disease. […]